Heart Attack – acute myocardial infarction
The essence of diagnosis of heart attack (acute myocardial infarction)
- Acute myocardial infarction is sudden severe pain in the front of a chest, which leads to hypotension and shock.
- Acute myocardial infarction is rarely painless, masquerading acute congestive heart damage, syncope, cerebral thrombosis, or shock from “unexplained” reasons.
- Fever, leukocytosis, elevated sedimentation rate, increased SGOT and LDH within 24-48 hours.
- ECG: abnormal Q waves, prolonged ST segment, later symmetrical T wave inversion.
General understanding of heart attack (acute myocardial infarction)
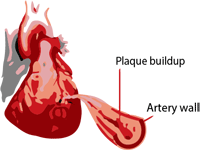
Acute myocardial infarction is the ischemic necrosis of one localized portion of the myocardium caused by coronary occlusion, due to the appearance of a thrombus, or atheromatous narrowing. To the occurrence of acute myocardial infarction comes and without a complete occlusion, if the flow in the coronary arteries are temporarily reduced, eg. in the postoperative or traumatic shock, or as a consequence of hypotension, or in the case of dehydration.
Myocardial infarction localization and duration depends on the anatomical distribution of blood vessels, the place of the current and previous occlusion and adequate supply of collateral circulation.
Thrombosis occurs most often in the front branch of left coronary artery and that results as a myocardial infarction of anterior wall of the left ventricle. Occlusion of the left circumflex artery leads to the anterolateral infarction. Thrombosis of the right coronary artery can lead to myocardial infarction of rear lower part of the left ventricle.
The clinical picture of heart attack (acute myocardial infarction)
Symptoms of heart attack (acute myocardial infarction)
Warning pain – mostly in 1/3 of patients, changes in the image of angina, sudden attack of atypical angina, or unusual changes in relation with digestion, which you can feel in your chest, acute myocardial infarction is going to happen within a few hours, days or weeks.
The pain of a acute myocardial infarction – could start during the rest time (even in sleep) or during activities. He is similar to anginal pain at the site and spread, but he is much stronger, with a resting he does not stop, and rapidly increases to the maximum strength, he can cause a death if he last more than a few minutes or longer. The pain can lasts for hours and often is unbearable. The patient wakes up in a cold sweat, feel weakness, turn himself, looking for a comfortable position. The patient who have acute myocardial infarction does not want to lie still. The following problems can occur alone or combined: mild headache, syncope, dyspnea, orthopnea, coughing, shortness of breath, nausea or vomiting and meteorism.
Painless acute myocardial infarction occure in 5-15% of cases, pain is absent or small and concealed by immediate occurred complications, visible acute pulmonary edema, or rapid heart damage, pronounced weakness, shock, syncope, or cerebral thrombosis.
Signs of heart attack (acute myocardial infarction)
Physical signs are very different, obvious clinical symptoms of attack and strength are not in correlation with the duration and localization of acute myocardial infarction.
Shock has been described in cases where the blood pressure is below 80 mm Hg (or higher, if there is hypertension), a pale face color, mental depression, cold and sticky skin, peripheral cyanosis, tachycardia or bradycardia and a weak pulse. Shock occurs only in severe attacks of acute myocardial infarction in 8-14% of cases. To shock comes primarily because of the pain, rather than the hemodynamic effects of heart attacks, visible improvement occurs within 30-60 minutes after the easing of pain.
In severe attacks of acute myocardial infarction the first and second heart sound are weakened, often vague. Often there is an accelerated rhythm and varicose veins in the neck. Picture is dominated by acute pulmonary edema and congestive heart damage. In light attacks of acute myocardial infarction, finding during the examination is normal, or reduced intensity of the first tone, and there is low systolic blood pressure.
Temperature does not appear in the acute myocardial infarction as well as during the prolonged state of shock. It usually grows to 37.8 and 39.4 ° C (100-103 ° F) rarely up to 40.6 ° C (105 ° F) within 24 hours and is held up to 3-7 days.
Laboratory findings of acute myocardial infarction are: leukocytosis are 10-20 thousand leukocytes. It usually occurs on the second day, and disappear after a week. The attack have a normal sedimentation rate, increasing the second or third day and remained elevated 1-3 weeks. SGOT activity is increased in the first 6-12 hours, has a top point after 24-48 hours and returns to normal after 3-5 days. Lactic acid levels remain increased 5-7 days.
ECG of heart attack (acute myocardial infarction)
ECG changes of acute myocardial infarction are not in good correlation with the volume of clinical picture of the stroke. The characteristic image consists of specific changes that pass in stereotypical “evolution” in a few weeks. In the acute myocardial infarction there is elevation of a ST segment and T waves and abnormal Q waves, ST segment later can be returned to its place and the T wave becomes symmetrically inversed. Correct diagnosis of acute myocardial infarction based on ECG can be solved only by the presence of all three changes. Serial STT segments by themselves are sufficient, but not with the diagnostic point of view. You can not see characteristic changes when there is left bundle branch block.
Complications of heart attack (acute myocardial infarction)
Congestive heart damage and shock occurs in heart attack, and stroke can develop insidiously or abruptly, with arrhythmia or pulmonary embolism. Every day, distension of the neck veins, a fast rhythm, the murmur of mitral regurgitation, abnormal pulsations of the heart, sensitive and painful enlarged liver and sacral edema should be treated.
If you do not being treated with anticoagulants, in 10-20% of cases, because of fleabite legs or pelvic veins, comes to the pulmonary embolism. This is characteristic of the acute and convalescent state.
Arrhythmia occurs after acute myocardial infarction and is considered to be the cause of death in 40% of patients. The mechanism is consists of either cardiac arrest or fibrillation of chambers, which occur after a shock or damage to the heart, and later there is a tendency to be the primary cause of death. Continuous monitoring can reveal the presence of ventricular tachycardia, complete A-V block and other less serious arrhythmias. Ventricular premature beat later can often lead to far more serious arrhythmias, but not early on primary ventricular fibrillation. It is important to recognize arrhythmia on time in order to initiate the therapy.
Cerebrovascular changes can occur due to a drop in blood pressure generated by myocardial infarction or embolism occurred because of the mural thrombus. It is advisable to take ECG from all patients with cerebrovascular changes.
Acute myocardial infarction recurred in 5% of patients, or it is manifested by prolonged state of myocardial infarction after the first attack. Rupture of the heart is not common. If it comes to rupture of the heart, it usually happens in the first week.
Perforation of the interventricular septum in acute myocardial infarction is very rare. It is characterized by the sudden appearance of a loud and rough systolic murmur because of acute myocardial damage. This have to be distinguished from mitral insufficiency caused by infarction or papillary muscle dysfunction. Both lead to heart damage and they require surgical intervention to the heart. Previously, patient’s condition needed to stabilize within a few weeks or months, and right and left heart catheterization have to be done, that could possibly show significant hemodynamic changes.
Early after convalescence, ventricular aneurysms and peripheral arterial embolism can occur. Approximately 20% of patients of acute myocardial infarction develop some kind of aneurysm, or left ventricular weakness, which are clinically recognized by abnormal paradoxical precordial pulsations. Some of these patients come into a state of refractory heart damage and surgical intervention is the only help.
Shoulder-hand syndrome occurs after prolonged immobilization of arm and it is caused by “reflex sympathetic dystrophy”. Are rarely can be prevent. Early pain over the injured shoulder accompanied by pain in hands, swelling and weakness of the hands and excessive sweating. If state of shock persists, there is oliguria, anuria and tubular necrosis.
Prognosis for heart attack (acute myocardial infarction)
The overall mortality during the first month after acute myocardial infarction is approximately 30%. The greatest number of deaths occurring in the first 12 hours. Clinically severe acute myocardial infarction for full recovery requires 6-12 weeks. Mortality increases with prolonged state of shock, severe heart failure, leukocytosis over 25 000 with eosinophilia, fever over 40°C (104°F), uncontrolled diabetes mellitus, the already existing heart attack, especially if the above factors are combined. Pulmonary embolism which is not treated with anticoagulants, during persistent arrhythmia, during prolonged myocardial infarction, and during early recovery mortality is 15-20%.
Long-term survival is depending on the ability of medical care and the presence of other chronic diseases. Complete clinical recovery allows 10-15 year life after acute myocardial infarction. Patients with signs of heart failure, arrhythmia and angina die within 3-6 years.
You may also like:
- Echocardiography
Echocardiography or heart ultrasound is a noninvasive, painless method and does not require any special preparations.
- Arteriosclerosis | Arteriosclerotic heart disease
Arteriosclerotic heart disease or coronary artery atherosclerosis is the most common underlying cause of cardiovascular events and death.
- All you need to know about hypertension or high blood…
One stop station for questions about hypertension or high blood pressure.