Rheumatic fever
When a person is infected with streptococcus bacteria, that can caused inflammation called rheumatic fever. In the beginning the patient suffers only from strep throat, and in most people this does not develop into serious consequences, but if it is untreated, the body begins to defend himself and that can cause inflamed and swollen brain, joints, skin and heart to stop beating. This inflammation can cause scars on the heart valves, that later can develop into rheumatic heart disease. Just a little number of patients with streptococcal infection or strep throat are likely to develop rheumatic fever. When rheumatic fever is cured she does not leave any effects on the brain, joints or skin, but only has consequences on the heart.
Criteria for diagnosis of rheumatic fever
Important sign of the rheumatic fever
- Carditis
- Sydenham chorea
- Subacute nodules
- Erythema marginatum
- Polyarthritis
Minor signs of the disease:
- Temperature
- Polyarthralgia
- Prolonged P-R interval
- Increased sedimentation rate or C – reactive protein.
- Evidence of previous beta hemolytic
- Streptococcus infection
Evidence of previously healed rheumatic fever or rheumatic valvular disease.
Diagnosis of rheumatic fever can be set if there are at least 2 or more major signs of the disease. Although early signs of rheumatic fever also can be rheumatoid arthritis, neurocirculatory dystonia, bacterial endocarditis, collagen disease and chronic infectious diseases.
General characteristics of rheumatic fever
Rheumatic fever is an acute or chronic system disease, which for unknown reasons may gradually bring up deformation of the heart valves. Rarely, can have acute and violent form.
Rheumatic fever is the most common cause of heart disease in people under 50 years of age. According to the general problems can be classified as a third disease, after hypertension and atherosclerotic coronary disease. Rheumatic fever happiness little more in men than in women, but the chorea is more common in women. Mostly appears in the age between 5 and 15, rheumatic fever is rare in children younger than 4 years and people after the 50s.
Rheumatic fever begins with hemolytic streptococcus infection and usually occurs 1-4 weeks after tonsillitis and otitis.
In the acute phase of rheumatic fever endocardium, myocardium, pericardium, lungs and pleura can be implicated. Characteristic changes are manifested in the form of perivascular granulomatous reaction, and vasculitis. Mitral valves were affected in 75-80% of all cases, the aortic valves in 30%, tricuspid and pulmonary valves in less than 5% of all cases. On the surface of edematous valve can come to the appearance of small red granules. They can be a complete cured. Progressive changes on the skin, that can result from acute or chronic inflammation, can be developed through months or years.
The clinical picture of rheumatic fever
Major signs of the rheumatic fever
Carditis findings can be used for diagnosis of rheumatic fever in cases where: In history we have data on rheumatic fever or valvular disease on rheumatic basis. If we know that in the past 4 weeks, there was a streptococcal infection of the upper respiratory tract.
- Carditis usually occurs in childhood at a very young age, in adults it is easier to detect with a series of ECG analysis. Presence of carditis can be established through any of the diseases listed below:
- Pericarditis with precordial pain or in epigastric of left shoulder, pain in the joints during movement. Characteristic changes in the ST segment of the ECG findings and presence of liquids to any degree. Pericarditis is frequently present in adulthood. Diagnosis can be set with a series of radiographs, they can show progressive increase of cardiac shadow.
- Increased heart, which can be diagnosed by physical examination and radiographs goes in favor of inflamed joints and myocardium. With a series of x-rays it is possible to detect changes in the size of the heart.
- Congestive heart failure. Decompensation of the right side of the heart is more pronounced in children. Painful and enlarged liver is an important sign.
- Mitral or aortic diastolic murmur speaks in favor of expansion of valvular ring or myocardium with or without associated valvulitis. In the absence of any of listed above signs, diagnosis of carditis dependent upon the following less specific changes in relation to the overall clinical picture.
ECG of rheumatic fever
ECG: the most important changes are prolonged P-R interval of more than 0.04 sec. Less specific changes in the contour of the P wave and T wave inversion.
Changes in the quality of heart sounds.
Pansystolic murmur at the top of the heart that persists or gets louder during the disease. Carey Coombs high diastolic murmur can be heard.
The rapid rhythm above third tone is difficult to differentiate among children and in patients in juvenile age.
Sinus tachycardia exists regardless of volume and degree of temperature. Remains during sleeping and significantly increases even with the lowest activity.
The next two characters usually appear to be associated with carditis, so there are a low value for the diagnosis of diseases in the beginning. However, occasionally can appear before carditis, and can be strong evidence for the existence of the rheumatic fever.
- Erythema marginatum is often associated with skin nodule. Changes begin with a fast increasing macula, and with the edge of the ring, or with a clear center. They can be easily enlarged or confluent. Skin rash may be short term or persist for a long time.
- Subcutaneous nodules – are rare, except in the children’s age. Few or more can be find, they are usually small, 2 cm or less in diameter, hard, insensitive, and there are attached on the fascia or tendons, such as the high profile joint on the elbow, on the dorsal side oh the hands, on the malleolus, vertebra and occipital bone. There are usually recurring and are difficult to clinically distinguish from nodules of rheumatoid arthritis.
Sydenham chorea – may occur suddenly as a totally isolated case or can be developed as part of rheumatic fever. It may be that in 50% of cases, there are other signs of rheumatic fever. Girls suffer more, and rarely occurs in adults. Chorea is accompanied by constant purposeless movements of the limbs, body and fascial muscular. There are often unspecified grimacing facial movements. These movements are aggravated by emotional excitement, and completely disappear during sleep. These episodes can last for weeks and sometimes even months.
Arthritis encountered in rheumatic fever is characterized by migrating pain, which occurs gradually or suddenly attacks large joints. Joints become hot, red, swollen and tender, while the inflammation in previously affected joints is easing. Body temperature increases progressively with changes in inflamed joints. In adults one joint can be affected or more smaller joints. Acute arthritis lasts for 1-5 weeks and stop without leaving deformations. Affected joints are among the more important sign of disease, but only in cases where there is fluid and signs of inflammation. This is the opposite of arthralgias, where there is a pain and braking, but without these objective signs.
Arthritis and arthralgia are common in childhood and younger age, and they are accompanied by fever and increased sedimentation. Streptococcal infection and throat problems are also often seen. Coincidentally these factors, combined, are confirming the diagnosis of rheumatic fever. Final diagnosis requires additional manifestations such as carditis or rheumatic manifestations such as erythema marginatum or chorea.
Less important characteristics of rheumatic fever
- Temperature is always accompanied arthritis and carditis. In the subacute and chronic phase, temperature is lower, and may be continuous or reccurent. Temperature is important only as evidence of the inflammatory process. Children and even adults can have a temperature of 37.5 to 37.8 ° C (99.5 to 100 ° F). This should not be interpreted as a temperature.
- Discomfort, stenia, weight loss and anorexia can be manifested as signs of only rheumatic process, but are also characteristic of other chronic diseases.
- There is a frequent abdominal pain. Often change the position and strength, and sometimes abdominal pain may lead to unnecessary laparotomy.
- Abdominal pain can occur due to an enlarged liver, rheumatic peritonitis, or rheumatoid arthritis, or may be transmitted from the pleural or pericardial. Pronounced pain in the joints, and in periarticular tissue, can also be symptoms of rheumatic fever.
Laboratory analysis of rheumatic fever is useful for three reasons:
As a non-specific information about inflammation, sedimentation is almost always increased during active rheumatic fever, except when chorea is the only clinical sign. There may be variations in the number of white blood cells, and there is a normochromic anemia. Proteinuria is occasionally found, but these findings do not suggest glomerulonephritis. There is also a streptococcal infection.
High titer or increased antistreptolysin titer go in favor of fresh infection, but this is not confirming existence of rheumatic fever. Culture swabs from the throat can extracted beta-hemolytic streptococcus in 50% of cases, when it comes to rheumatic fever.
Hard evidence against diagnosis is low presence of anti-streptolysin O titer (50 Todd units) that does not increase by the repeated testing. In the case of active rheumatic fever the sedimentation is rarely normal.
The differential diagnosis of rheumatic fever
The differential diagnosis covers following diseases: rheumatoid arthritis, osteomyelitis, traumatic injuries of joints, neurocirculatory stenia, cardiac neurosis, bacterial endocarditis, pulmonary tuberculosis, acute poliomyelitis, disseminated lupus erythematosus, serum disease, leukemia, sickle cell anemia, inactive rheumatic heart disease, congenital heart defect and “surgical abdomen”.
Prognosis for rheumatic fever
Incubation of rheumatic fever in children last for months and weeks in adults. In the span of 5 years, about 20% of the children can get reinfection. However, the infection can not be repeated often if the patient is feeling well for 5 years or more, and rheumatic fever is rare after 21 years of age. Early mortality is 1-2%. If rheumatic activity persist and in addition there is a very enlarged heart, then cardiac decompensation, and pericarditis, then the prognosis is poor, it is considered that 30% of children with these changes die within 10 years from the beginning of the first attack. Eighty percent of patients experience a mature age, and half of them have little or no limitations in life activities.
After the first attack, about 1/3 of young patients have problems with heart valves, usually a combination of mitral stenosis and insufficiency. After 10 years in 2/3 of patients have valvular heart disease. In adults, heart damage occurs in less than 20%. Mitral insufficiency is the most common, and aortic insufficiency is more frequently presented in adults than in children.
You may also like:
- Aortic stenosis clinical picture and treatment
Aortic stenosis is a chronic rheumatic heart disease that creates rigidity and deformation of the heart valves. Aortic stenosis can be prevented.
- Cardiac tamponade
Cardiac tamponade is a rare life-threatening complication in which there is accumulation of fluids, blood, clots, or gases in the pericardial space.
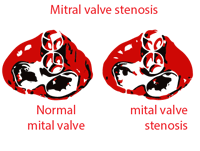
- Mitral valve stenosis
Mitral valve stenosis is a chronic rheumatic heart disease, leading to one or more attacks of rheumatic fever, which creates rigidity and deformation of the heart valves.